A global health challenge meets Marlborough-made technology
A visiting microbiologist from Senegal’s Institut Pasteur de Dakar was in Marlborough last week to work with local biotech company DNAiTECH on a portable diagnostic tool for measles — part of an international public health project funded by Grand Challenges Senegal and backed by Grand Challenges Canada.
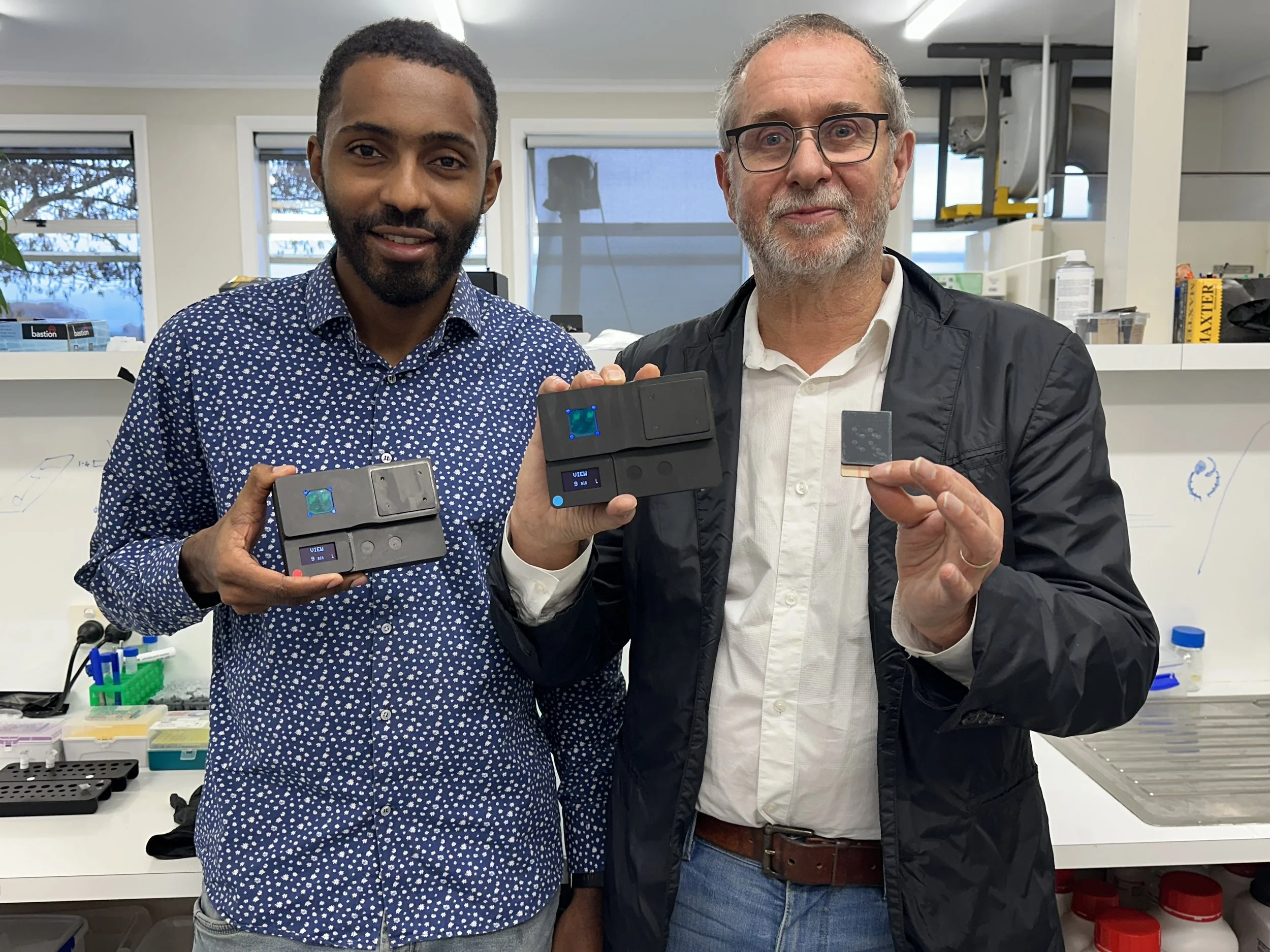
Microbiologist Andy Diouf from the Institut Pasteur de Dakar with DNAiTECH founder and CEO Murray Broom.
The collaboration between DNAiTECH from its office at the Marlborough Research Centre’s Grovetown Park and the Institut Pasteur de Dakar began in mid-2024, with DNAiTECH contracted to develop a portable molecular testing platform for use in West Africa. Microbiologist Andy Diouf’s visit was a critical step ahead of clinical field trials scheduled to begin in Senegal this September.
“Our goal is to develop a tool that can be deployed at the point of care — sensitive, specific, and easy to use for detecting measles,” says Andy. “DNAiTECH has done a great job.”
Tackling Measles — and more
Measles remains a serious public health threat in parts of Africa. While it has been eliminated in many countries, outbreaks continue in regions where vaccination rates have dropped — especially after the COVID-19 pandemic. Early detection plays a key role in stopping transmission, but current methods can be slow, with samples needing to be shipped to central labs in Dakar.
The solution being developed by DNAiTECH is designed to solve that. Their portable, battery-powered device uses a diagnostic chip — about the size of a credit card — to detect measles through its genetic signature.
Because measles and rubella can cause similar symptoms, particularly in children, the test was designed to detect both viruses.
“You can’t tell them apart just by looking at a rash,” says Andy. “But one — measles — is far more contagious and dangerous. That’s why the chip is programmed to ask both questions and that’s what makes the technology so very interesting.”
From sample to diagnosis — without a lab
What makes DNAiTECH’s platform distinct is its portability and field-readiness. The molecular test doesn’t require refrigeration, mains power, or a full lab — just the battery-powered handheld device and chip.
“With molecular diagnostics, we look directly for the virus’s genetic material,” explains DNAiTECH founder and CEO Murray Broom. “Our system amplifies the viral signature, even at very low levels — making early detection possible.”
Serology-based tests, which detect the body’s antibody response, often take much longer after infection to show results. “By the time antibodies are present, the outbreak could already be spreading,” says Andy. “That’s why this approach is so valuable.”
Testing in Marlborough for trials in Senegal
Over two weeks in Marlborough, Andy has worked alongside DNAiTECH’s team to learn about the technology and to provide his feedback for the realities of the Senegalese climate. He brought extracted RNA from patient samples to help validate the tool and shared insights into deploying diagnostics in high-humidity, tropical environments.
“Our reagents must remain stable without a cold chain,” says Murray. “We’ve developed a proprietary system where the chemistry is embedded in a dry, absorbent material — it’s robust, transportable, and activates at the point of care.”
Even the sample preparation device — a syringe-style tool that extracts and purifies viral RNA — is designed to work without mains power.
Yellow Fever: a new project in the pipeline
Following progress on the measles tool, DNAiTECH was approached by Dr Oumar Ndiaye from the Institut Pasteur de Dakar to explore a similar solution for yellow fever — a mosquito-borne virus that continues to cause outbreaks in tropical regions of Africa, South America, and Asia.
Like measles, yellow fever is vaccine-preventable — but inconsistent vaccine availability means it remains a threat in many communities.
“These diseases are often overlooked by Western diagnostic companies,” says Andy. “But they’re still causing major public health problems. That’s why these tools matter.”
Because DNAiTECH’s device is a platform, the same system can be used to detect different viruses — simply by changing the chemistry on the chip.
Small team, global impact
At the Institut Pasteur de Dakar, Andy works among 600 staff across departments like virology, immunology, and vaccine development. In Marlborough, he’s been embedded in DNAiTECH’s four-person team — and appreciates the pace and focus.
“Because everyone’s working on the same project, we move quickly,” he says. “And Marlborough is beautiful — I love the town, the mountains, the peacefulness. It’s been a really positive experience.”
For DNAiTECH, the collaboration reflects their mission: creating revenue-generating technology with real-world social impact.
“We’re not trying to replace lab-based tools,” says Murray. “We’re building something different — something that works in places where labs don’t exist. That’s the whole point.”
As clinical trials begin next month, this Marlborough-made technology could soon be helping health workers across Senegal detect outbreaks sooner — and respond faster.